Infectious Disease Control and Architectural Design
Scroll Down
Clinical healthcare professionals and researchers from a variety of professions, including physicians, nurses and pharmacists in the field, as well as bacteriologists, continue the daily battle against the novel coronavirus (COVID-19) that is currently running rampant around the world. We spoke with Dr. Akira Ito, a member of the Building Services Design Division, Engineering Department which is regularly involved research on infectious disease control in medical settings, together with healthcare professionals.
CATEGORY
RELATED EXPERTISE
Team approach to infectious disease control
In addition, research activities are being developed to protect against and prevent the spread of infectious diseases not only in the clinical field, but by using a multi-faceted approach to control pathogenic bacteria and viruses, as a reliance on antibiotics to protect against and prevent the spread of such bacteria and viruses is simply not sufficient as antibiotic-resistant bacteria continue to emerge. Under these conditions, architects have joined teams of medical professionals and researchers to carry out research and put infectious disease control measures into practice in the field of architecture.
Architectural design that helps cut off infection routes
Infections take hold only when three factors converge: the existence of a pathogen (microbe causing an infectious disease), host (human in which a pathogen grows), and an infection route (transmission pathway that carries the pathogen). Hospitals are high-risk areas where all three factors are present.
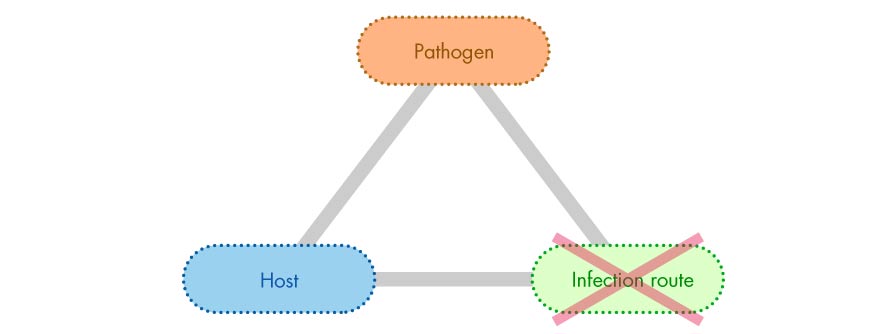 Pathogen x host x infection route
Pathogen x host x infection route
Types of infection routes and architectural design measures
“Contact transmission” is an infection route through direct or indirect contact with a patient. Measures to avoid this include “hand hygiene” and “environmental surfaces (surfaces touched by hands)” through innovations in architectural design.
Measures to avoid “respiratory droplet transmission” include the arrangement and layout of beds and furniture that consider the distance that droplets can reach (2m).
Primary measures for “air-borne transmission” include the use of private rooms for patients and “negative pressure ventilation” in which a steady flow of air is pumped into a hospital room based on the difference between supplied and vented air.
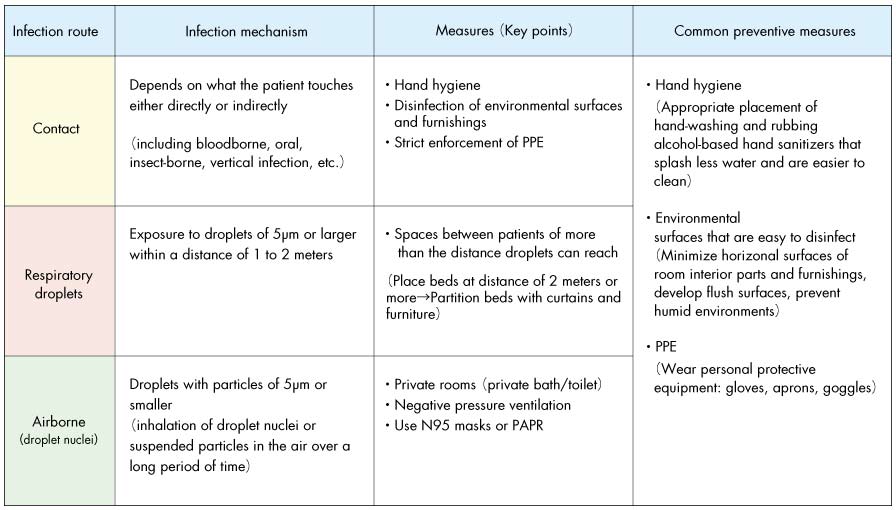 Healthcare-related infectious diseases and important points on measures
Healthcare-related infectious diseases and important points on measures
Points on controlling infections from planning to implementation
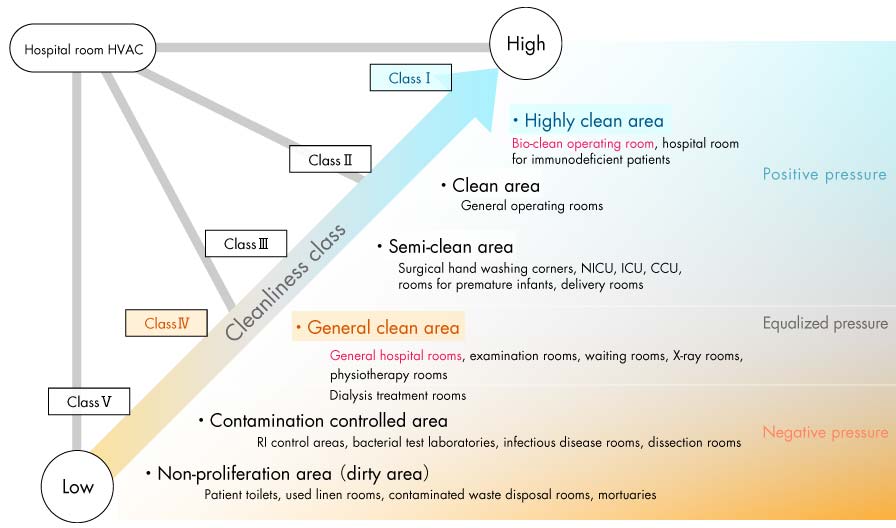 Air cleanliness classes and zoning in hospitals
Air cleanliness classes and zoning in hospitals
(Created by the author based on “Guidelines for Design and Management of Hospital HVAC (HEAS-02-2013)” published by the Healthcare Engineering Association of Japan (HEAJ), 2013)
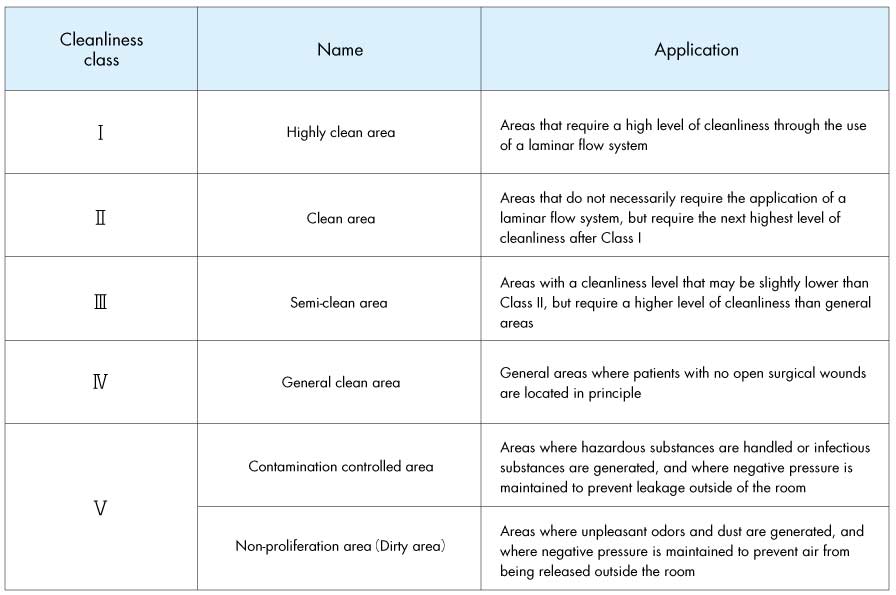 Air cleanliness classes in hospitals
Air cleanliness classes in hospitals
A brief explanation follows on planning requirements and important points on infection control.
①Creating a safe flow of air: Airborne Infection Isolation Room (AIIR)
Conventional hospital plans often focus on temperature/humidity and air volume (ventilation frequency). However, safe air flow is designed in infection control measures from the perspective of “air pressure”, “air cleanliness”, “air flow method”, and “air flow distribution” in preparation for airborne infections.
For example, if a HVAC system can create a flow as shown in the following figure while also taking into account the balance between supplied and vented air, it will be possible to isolate the source of an infection and reduce the risk of infection for medical staff.
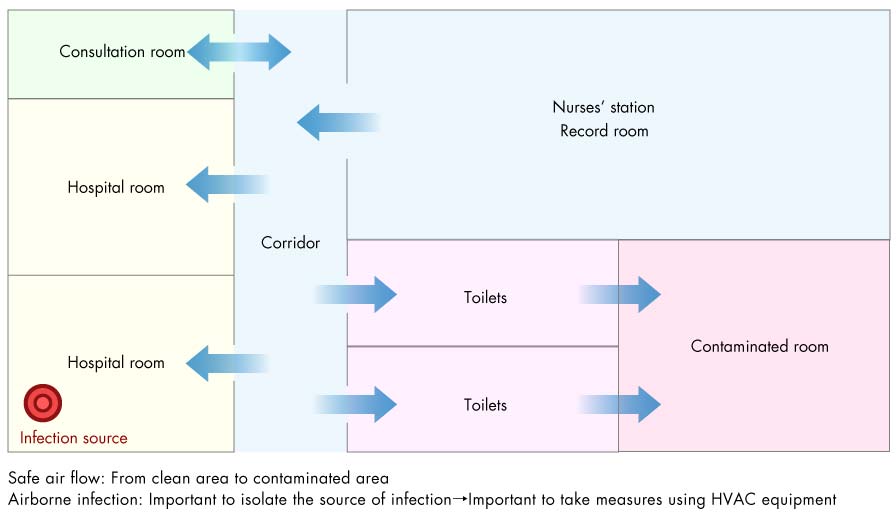 Air flow in hospital wing (example)
Air flow in hospital wing (example)
・Create a constant flow of air to hospital room and maintain a negative pressure of -2.5Pa
・Ensure air is ventilated frequently
・Use airtight specifications for interior materials
・Release contaminated are directly outside
・Use ultra-high performance air filters (HEPA filters) when air is circulated indoors
・Continuously monitor status of negative pressure
・Also effective to use hospital rooms with an anterior space to manage negative pressure
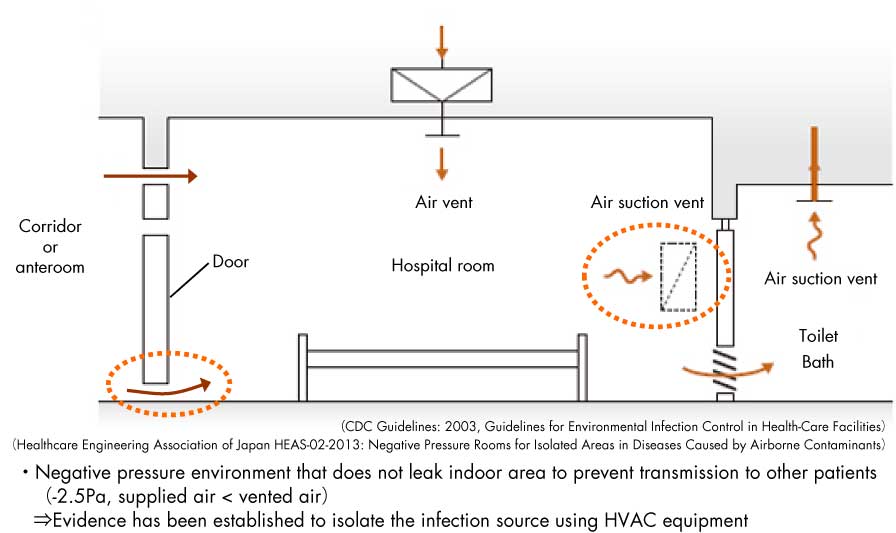 AIIR (Airborne Infection Isolation Rooms)
AIIR (Airborne Infection Isolation Rooms)
②Creating a safe flow of air: Protective environment (PE)
Rooms for patients with immunodeficiencies should have an airflow that is the opposite of that in an AIIR. In other words, contaminated air should never be allowed to enter the room. Therefore, to create a PE, measures are taken to set the environment of the hospital room to a positive pressure of +2.5Pa.
③Installation of easy-to-use hand hygiene systems
In order to ensure thorough hand hygiene to reduce the risk of infection through contact, it is effective to clearly separate equipment and facilities by application and user, such as hand washing basins for patients, clean sinks for medical staff to use for hand washing, and sinks for washing contaminated equipment after use.
In addition, the installation of hand-washing equipment and facilities in several easy-to-use spaces will result in meticulous hand washing. Therefore, it is important to determine the location of these spaces after conducting a survey and analysis of the trajectory of behavior of medical staff.
Setting that consider the psychology of human behavior should also be considered, such as not installing mirrors around wash stands to encourage people to avoid the tendency to touch their faces when looking in mirrors.
④Creating an environment where microorganisms cannot multiply
Microorganisms multiply in humid spaces where water is abundant. For example, research is advancing on designs for hand washing in which water does not splash or pool around edges. External insulation is also effective in preventing water droplets from forming due to condensation, as well as the use of antimicrobial air conditioners.
Toilet drainage pipes were identified as likely routes of transmission during the SARS outbreak. It is also necessary to adopt designs that use traps for drained water with low levels of air leakage for drainage routes where microorganisms can grow easily.
⑤Environmental surfaces where it is difficult for dust to accumulate and is easy to sterilize and clean
It is important that environmental surfaces (room elements, furniture, fixtures, etc.) are easy to disinfect and clean and difficult for dust to accumulate. This may include, for example, designing areas where the walls and floors intersect as curved structures, installing air conditioners and trash cans on the walls so that dust does not accumulate on the floor surface, tilting the top surfaces of furniture, and adding casters to furniture so that they can be moved around when cleaning. Pathogens are mostly transmitted from environmental surfaces to patients when hands come into contact with these surfaces, so it may not be necessary to compulsively disinfect/sterilize areas that will not come into contact with hands.
The use of non-contact systems, such as automatic faucets and cleaners that use sensors, is effective since there is no direct contact with water around where pathogenic bacteria can easily grow.
⑥Avoid excessive infection control that is not based on evidence (scientific based)
For example, in the past, medical professional changed their shoes before entering an operating room. However, as mentioned above, infections transmitted through contact are known to occur mostly through the hands, so the risk of infection from feet is believed to be extremely low. Planning based on scientific evidence, regardless of past hygienic practices and cultures, will allow the necessary space and flow lines to be secured and result in a higher quality of medical care.
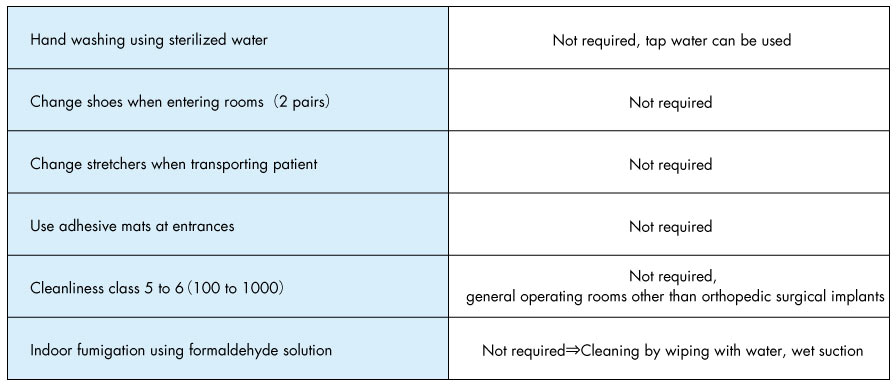 Habits, cultures and lack of common sense in the surgery department?
Habits, cultures and lack of common sense in the surgery department?
⑦Precautions during construction
Aspergillus fungal spores are a type of mold found in dust, such as in the ceilings of buildings.
When a person who is immunodeficient becomes infected with this mold, it can cause a severe respiratory infection. When renovation work is being carried out at an existing hospital with patients that have compromised immune systems, care must be taken to ensure that curing, negative pressure ventilation, and proper ventilation areas are in place to thoroughly contain dust from construction work.
In addition, it is also necessary to consider infection control risk management, such as separating the flow of workers from patients and sampling microorganisms, as well as keeping patients away from the construction site.
Development of technology and “visualization” of infectious disease control
Evidence can be obtained from the early stages of hospital planning to create safer airflows, achieving the design and operation of hospital rooms that take patient safety and reducing the risk of airborne infections for healthcare professionals into account more than ever.
I would like to continue researching how the architectural field can contribute to addressing the fear of infectious diseases in the future.
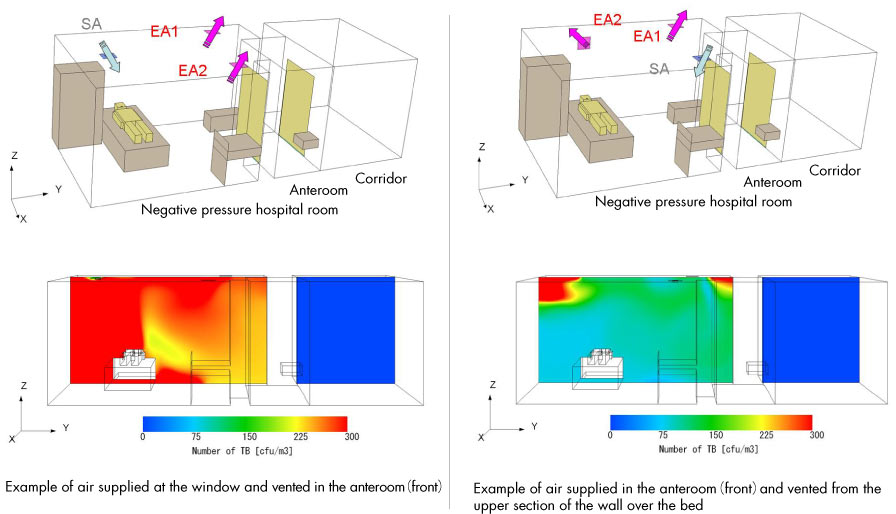 Simulation of airflow in AIIR (negative pressure room) (computational model, distribution of droplet nuclei)
Simulation of airflow in AIIR (negative pressure room) (computational model, distribution of droplet nuclei)